The potential benefits of precision medicine also come with new challenges.
Importantly, the amount and complexity of data available for each patient is rapidly increasing.
How will clinicians figure out which data is useful for a particular patient?

What is the most effective way to interpret the data for go for the best treatment?
These are precisely the challenges thatcomputer scientists like meare working to address.
Randomized controlled trialsrandomly place participants in different groups that receive either an experimental treatment or a placebo.
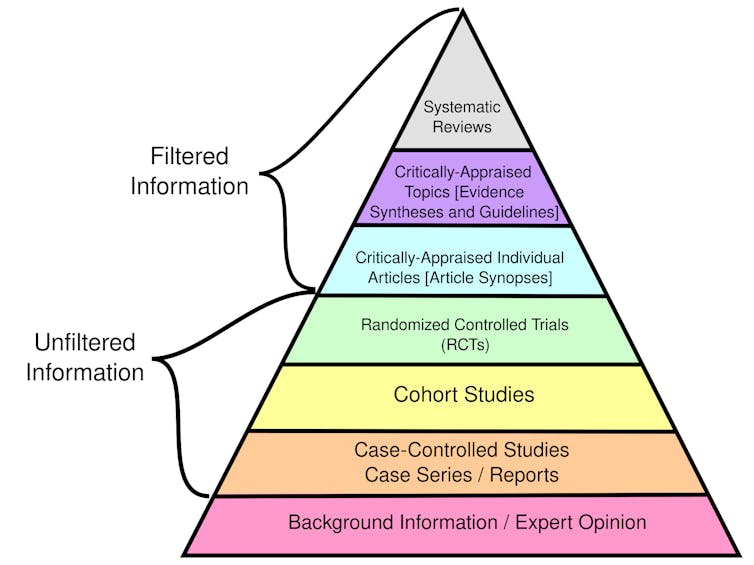
Overall,systematic reviewsthat synthesize the findings of multiple research studies offer the highest quality evidence.
Similarly, personal testimonials and expert opinions alone are not supported by empirical data.
Integrating evidence, patient preferences and their own expertise, they can develop diagnoses and treatment plans.
As may be expected, gathering and putting all the evidence together can be a laborious process.
These guidelines provide recommendations and standards of care based on systematic and thorough assessment of available research.
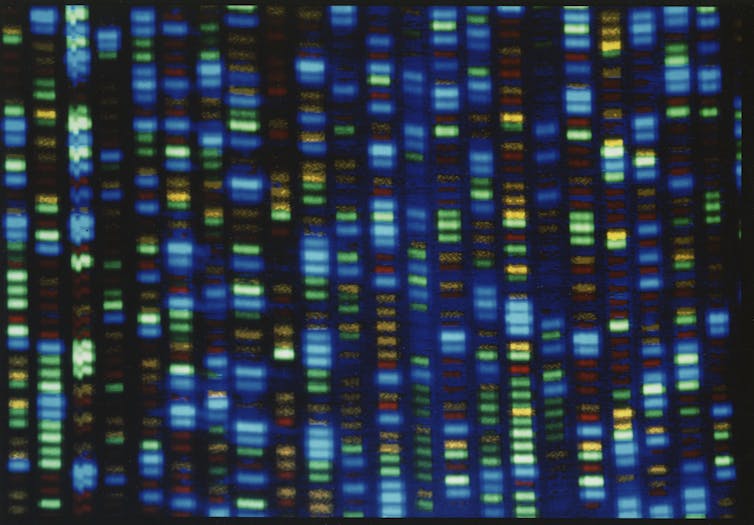
The first was theHuman Genome Project, which officially began in 1990 and was completed in 2003.

Increasingly, clinicians areanalyzing a patients DNAto identify genetic variations that inform their care.
The second was the development ofelectronic medical recordsto store patient medical history.
Adoption did not become widespread until after the 2009American Recovery and Reinvestment Act.
For example, some genes can affect how well certain medications work for different patients.
Another example is diagnosingrare diseases, or conditions that affect fewer than 200,000 people in the U.S. Related studies are already producing promising results inprecision oncologyand personalized preventive health.
These developments will significantly alter how clinicians make decisions and provide care over the next 50 years.